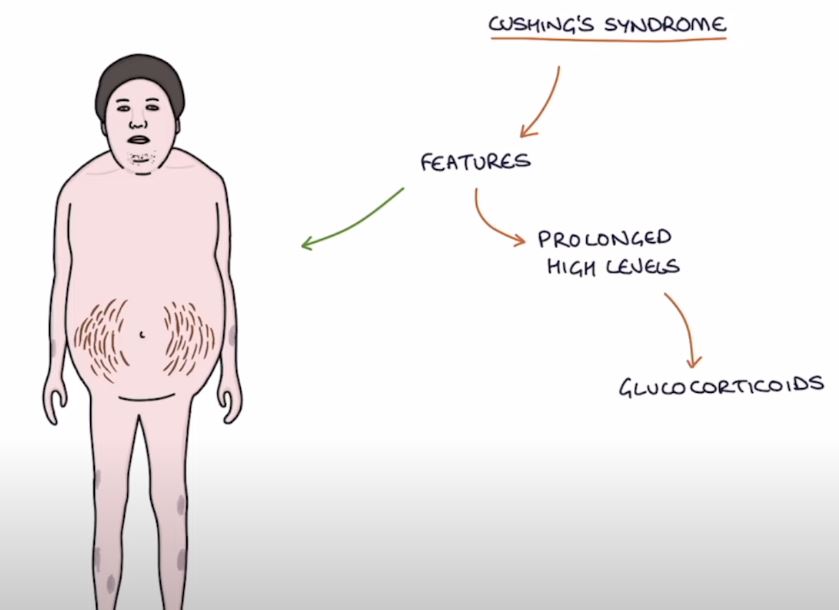
Cortisol is a key player in the complex hormonal orchestra that controls the human body. It regulates blood pressure, blood sugar, and even our response to stress, much like a conductor keeps the beat. But that delicate rhythm degenerates into chaos when Cushing’s disease enters the picture. This disorder, which is brought on by a benign pituitary tumor, causes persistently high cortisol levels, which can cause symptoms that are frequently confused with stress, aging, or weight gain.
Endocrinologists have made significant progress in diagnosis and treatment outcomes over the last ten years. They can now detect the condition more quickly and accurately by combining hormone assays, MRI scans, and dexamethasone suppression testing. The emotional toll on patients who previously wandered through years of misdiagnosis has been greatly lessened by this speed up in diagnosis.
Cushing’s Disease Key Facts
| Feature | Details |
|---|---|
| Name | Cushing’s Disease |
| Underlying Cause | ACTH-secreting pituitary adenoma (non-cancerous tumor) |
| Main Hormonal Effect | Excess cortisol production from adrenal glands |
| Classic Symptoms | Moon face, buffalo hump, stretch marks, central obesity |
| Systemic Symptoms | Anxiety, muscle weakness, osteoporosis, vision changes |
| Diagnosis Tools | Dexamethasone test, MRI, 24-hour urinary cortisol, salivary cortisol |
| Primary Treatment | Transsphenoidal surgery to remove pituitary tumor |
| Additional Therapies | Radiation therapy, hormone-blocking drugs, adrenalectomy |
| Success Rate (Surgery) | 65–90% (microadenomas); lower in macroadenomas |
| Reference | Mayo Clinic – Cushing’s Disease |
An Invisible Saboteur: When the Pituitary Gland Overreacts
Many patients experience a subtle beginning to their journey, such as a slight increase in weight around the midsection, unusual exhaustion, or unexplained skin bruises. Despite their apparent innocuousness, these symptoms are some of the first indications of something deeply hormonal. As time passes, more obvious characteristics appear, such as a round face, a fatty deposit between the shoulders, and purple stretch marks that dermatologists believe are especially suggestive of systemic hormone imbalances.
Cushing’s disease has an exceptionally misleading profile when viewed in the context of chronic illness. It often goes undiagnosed because it mimics more common conditions like depression, type 2 diabetes, or high blood pressure. An endocrinologist saw the classic “moon face” and ordered a midnight cortisol test after a woman in her early forties complained of chronic fatigue and facial swelling, which she attributed to stress. Her life was altered by that straightforward blood draw.
Identifying a Quiet Illness: Accurate Instruments and Skilled Eyes
Solving a hormonal riddle is similar to diagnosing Cushing’s disease. Endocrinologists frequently combine information from bloodwork, 24-hour urine samples, and pituitary imaging because no single test can give a comprehensive picture. The dexamethasone suppression test, which determines whether cortisol levels react appropriately to synthetic steroids, is one of the most informative of these.
Clinicians have been able to distinguish Cushing’s disease from other causes of hypercortisolism, such as adrenal tumors and ectopic ACTH production, by using sophisticated imaging tools and hormone sampling techniques. Diagnostic accuracy has significantly increased as a result of strategic partnerships between radiologists, endocrinologists, and neurosurgeons, allowing for quicker interventions and better results.
A Surgical Attack: Eliminating the Hormone-Happing Tumor
Surgery becomes the first line of treatment after a diagnosis. Patients with identifiable pituitary microadenomas have shown remarkable success with transsphenoidal surgery, a minimally invasive procedure that accesses the tumor through the nasal cavity. This method, which is carried out by skilled neurosurgeons, removes the tumor precisely while preserving healthy tissue.
Remission rates are higher than 80% in patients with small, well-localized tumors. However, the chance of a full recovery is greatly diminished when tumors are larger or invisible on imaging. In these situations, targeted medical treatments, radiation therapy, or another surgery are frequently advised.
Life Following Pituitary Reset: Symptoms of Recovery
Cortisol levels frequently plummet after surgery, which is a positive sign but necessitates cautious hormone replacement. Steroid support is progressively reduced during this phase to give the body’s natural regulatory systems time to recover. In the end, it’s a process that restores emotional equilibrium and a sense of vitality, but it takes time and support.
Physicians track cortisol recovery and screen for potential recurrence through regular follow-ups. The majority of patients report significantly better sleep, blood pressure that has stabilized, and—above all—a feeling of having control over their own bodies again.
When Surgery Is Insufficient: Support from Medicine and Radiology
Pharmacologic therapy is used for patients who cannot have surgery or whose illness does not improve. Mifepristone, metyrapone, and ketoconazole are among the medications that are especially helpful in lowering cortisol levels. These drugs provide symptom relief and serve as stopgap measures for more permanent treatments like radiation therapy or adrenalectomy, but they are not curative.
In extreme situations, bilateral adrenalectomy can save lives, but it is rarely the first choice. However, it increases the risk of Nelson’s syndrome, a condition in which the pituitary tumor grows more aggressively due to a lack of cortisol feedback, and requires lifelong hormone replacement.
The Hormonal Battle’s Emotional Terrain
Living with Cushing’s disease is a psychological journey that involves more than just the physical symptoms. During the diagnostic phase, many patients report feeling as though they have lost their identity, confidence, and vitality. However, following treatment, a remarkable level of resilience is revealed. Support groups—especially online forums—have developed into lifelines, places where people can turn their loneliness into strength through shared experiences.
A teacher who was diagnosed with Cushing’s disease after a two-year delay shared a heartwarming story about how the surgery restored her health and rekindled her ability to relate to her students. “I no longer felt alienated by my own body,” she remarked. Small victories along the way, such as walking to work once more, during her recuperation serve as a testament to the adaptability of people and the advancements in modern medicine.
At the Hormonal Frontier: Innovation
It is anticipated that Cushing’s disease treatment will undergo significant change in the upcoming years. The next generation of interventions will be much quicker, safer, and more individualized by combining wearable cortisol monitors, targeted ACTH blockers, and AI-driven hormone analysis.
A number of cortisol-modulating drugs are now in late-stage trials, demonstrating the acceleration of pharmaceutical innovation. These treatments seek to reverse damage as well as manage symptoms, especially to the skeletal and cardiovascular systems, which are most impacted by chronic hypercortisolism.