Sickle cell disease (SCD) is one of the most emotionally charged and medically complex conditions in the ongoing discussion about chronic illness and genetic inheritance. It affects families, communities, and entire healthcare systems; it is simultaneously a blood disorder and a sign of inherited heritage. Notwithstanding the difficulties it presents, SCD is beginning a remarkably optimistic phase, driven by advancements in science and the unwavering determination of those who live with it.
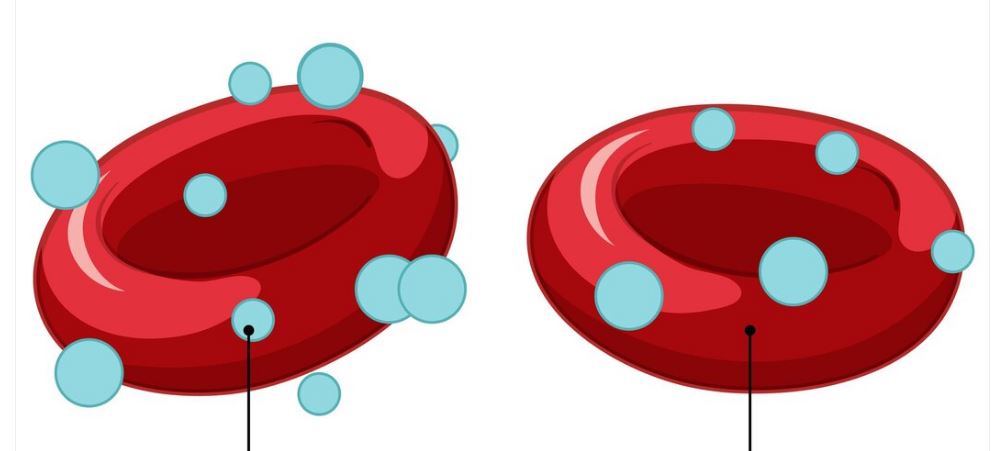
Red blood cells, the body’s most vital delivery system, are naturally changed into delicate, crescent-shaped agents of disruption by sickle cell disease. In most cases, red blood cells glide through vessels like pliable messengers. However, in sickle cell disease (SCD), these cells become sticky and rigid, clumping together and obstructing blood flow. The kidneys, brain, and lungs are among the vital organs that are harmed over time by this disruption, which frequently causes excruciating pain crises known as vaso-occlusive episodes.
Sickle Cell Disease Overview Table (WordPress Compatible)
| Key Area | Information |
|---|---|
| Condition Name | Sickle Cell Disease (SCD) |
| Underlying Cause | Mutation in the hemoglobin-producing gene (β-globin) |
| Primary Impact | Rigid, sickle-shaped red blood cells block vessels and reduce oxygen flow |
| Typical Onset | Symptoms usually begin by 6 months of age |
| Most Affected Populations | Predominantly people of African, Mediterranean, and Middle Eastern descent |
| Major Symptoms | Pain crises, fatigue, delayed growth, infections, vision problems |
| Complications | Stroke, acute chest syndrome, splenic crises, chronic kidney disease |
| Current Treatments | Pain management, blood transfusions, hydroxyurea, gene therapy |
| Recent Breakthroughs | FDA-approved gene-editing therapies (December 2023) |
| Reference Source | NIH – Sickle Cell Disease |
A Illness of Tradition—And Now, of Hope
Sickle cell disease stands out in the context of global genetics. Only when a child receives two mutated hemoglobin genes, one from each parent, does it become apparent. Carriers, who only have one copy, usually don’t have any symptoms, but they can unintentionally spread the gene. Because of this, early screening and genetic counseling are especially helpful, particularly in areas with a high carrier rate.
Healthcare practitioners have made significant progress in early detection over the last ten years, frequently detecting sickle cell through prenatal screening or newborn heel-prick tests. By all measures, these early interventions give people a leg up in the never-ending battle against health issues. Even though sickle cell disease is chronic and has an early onset, it does not determine a person’s fate. Many SCD patients are living longer, more fulfilling lives well into their 50s and beyond with the right care.
Coping with Emergencies: When the Blood Becomes Enraged
One of the most upsetting characteristics of SCD is the occurrence of pain crises, which are frequently abrupt and incapacitating. These are not your typical aches; rather, they are excruciating episodes brought on by obstructions in blood flow, which prevent oxygen from getting to the tissues. These crises can occur suddenly and last for hours or even days for many patients. Strong opioids, hospital stays, and intravenous hydration become commonplace.
It is so overwhelming that even slight pressure from a bedsheet can be intolerable, as one patient put it: “a burning sensation that radiates from the bones outward.” These testimonies are not uncommon; millions of people around the world incorporate them into their everyday lives.
Using Medical Innovation to Develop Resilience
Even though sickle cell disease is severe, it is no longer thought of as inevitable. Improvements in care have raised quality of life and drastically decreased mortality. For example, hydroxyurea has demonstrated remarkable efficacy in raising fetal hemoglobin levels, thereby decreasing the incidence of hospitalizations and crises. Another layer of support is provided by iron chelation therapy in conjunction with routine blood transfusions.
Gene therapy has taken a very positive turn and is now a ray of hope. Scientists can now alter the patient’s stem cells by incorporating gene-editing methods like CRISPR, either by adding a corrected gene or changing the defective one that already exists. These methods are not only groundbreaking in science, but they are also changing the perception of what it means to have a “genetic disorder.”
The Heroism of Living with Sickle Cell Disease Every Day
Sickle cell is an experience rather than merely a disease. Patients frequently exhibit incredibly touching resilience as they navigate adulthood with invisible pain or deal with school days disrupted by exhaustion. One adolescent who was diagnosed at birth described how he manages football practice, treatment, and tutoring younger children. Like many others, his story demonstrates how a generation is not only surviving but flourishing.
Through partnerships with educators, clinicians, and support groups, families are creating spaces where kids with sickle cell disease (SCD) don’t feel “different” but rather empowered. As a safeguard against the loneliness that chronic illness can occasionally cause, this emotional and psychological support is equally as important as medication.
Why There Is Still a Lack of Public Awareness and Why That Needs to Change
Results for medical conditions in their early stages are frequently influenced by visibility. Even though sickle cell disease affects more than 100,000 people in the United States alone, it still receives disproportionately little attention when compared to other genetic conditions. The figure rises into the millions worldwide, with Sub-Saharan Africa bearing the brunt of the burden.
These days, researchers and policymakers are working to alter this narrative through strategic alliances with advocacy organizations. Finally, awareness is growing by emphasizing the lived experiences of people with sickle cell disease and including patient perspectives in policy discussions. This change is not only long overdue, but also especially important.
A Prospective Perspective: Lifespan, Access, and Equity
It is anticipated that advances in gene therapy, along with earlier diagnosis and improved access to care, will greatly enhance results in the years to come. Comprehensive care, which includes regular eye exams, immunizations, and psychological support, has already been demonstrated in pilot programs to extend life expectancy and lower complications.
Organizations like the NIH and CDC are promoting change on several fronts by increasing research in underprivileged communities and utilizing digital health tools. And there is increasing hope that these advantages will go well beyond developed countries as global health collaborations grow in popularity.
One Cell at a Time: Redefining a Disease
Hospital beds and emergency rooms are no longer the only places where sickle cell disease is a silent burden. It is a cutting-edge problem in innovation, equity, and genetics. The future of sickle cell disease is becoming brighter—illuminated by science, strengthened by community, and sustained by hope—with every new discovery, patient story, and policy change.
Would you prefer this version to be more focused on current gene therapy case studies and clinical trials, or tailored for a regional audience such as those in the Caribbean, Nigeria, or the UK?